Lymphedema is a chronic condition characterized by swelling due to the accumulation of lymph fluid in an area of the body, most commonly in the arms or legs. When learning or reading up on lymphedema, the focus tends to be on cancer treatments, particularly those involving lymph node removal or radiation. However, secondary lymphedema can be caused by various non-cancer-related conditions or reasons. What are these causes, and are they treated any differently by a certified lymphedema therapist?
What is Secondary Lymphedema?
Lymphedema is classified as either primary or secondary. Primary lymphedema is caused by genetic or congenital abnormalities in the lymphatic system that someone is born with. Secondary lymphedema occurs due to damage to the lymphatic system from other factors. Although cancer is the most common cause of secondary lymphedema in the United States, it is not the most common worldwide.
Causes of Secondary Lymphedema (Non-Cancer Related)
1. Trauma and Injury
Severe injuries, such as fractures, burns, or deep wounds, can damage the lymphatic system. Once the system is damaged, it causes a backup of lymph fluid, leading to swelling in the affected area. Trauma-induced lymphedema can develop when lymphatic vessels are injured or destroyed, making it difficult for lymph fluid to drain correctly.
- Surgical Trauma: Procedures such as joint replacements, liposuction or other cosmetic surgeries, and vascular surgeries may accidentally damage lymph nodes or vessels, increasing the risk of lymphedema.
- Crush Injuries or Fractures: Accidents happen, but a significant injury can also involve damage or severe compression to the lymphatic vessels and limit lymph fluid circulation.
- Scar Tissue: Excessive scar tissue from an injury or surgery can clog and block lymph flow, trapping lymph fluid in an area.
2. Chronic Venous Insufficiency
Chronic venous insufficiency is a condition in which the veins in the legs weaken and struggle to return blood from the body to the heart. This is commonly seen with aging and often leads to swelling, skin color changes, and ulcers in more severe cases. Over time, the excess fluid overloads the lymphatic system, causing secondary lymphedema, which is often referred to as phlebolymphedema.
- Venous Hypertension: When an increased amount of blood is in the veins that are not moving back to the heart. This causes increased pressure in the veins, forcing fluid into the surrounding tissues and overwhelming the lymphatic system.
- Deep Vein Thrombosis: A blood clot can obstruct normal blood flow, leading to long-term swelling and other severe medical issues. If one suspects having a DVT, it’s essential to seek medical attention right away.
3. Infections
Infections and lymphedema can be good friends, unfortunately. As previously mentioned, in the US, the most common cause of secondary lymphedema is cancer and cancer treatment. The most common cause of secondary lymphedema worldwide is filariasis, a parasitic infection transmitted through mosquito bites—these damage lymphatic vessels and cause swelling and lymphedema. Additionally, recurrent bacterial infections can lead to lymphedema. The most common is cellulitis, which often causes lymphedema or worsens one’s condition if they already have it. Those with lymphedema are also at a higher risk of developing cellulitis due to the pooling of fluid in the area, and the body has difficulty fighting off these infections.
- Cellulitis and Infections: Bacterial infections in the skin can damage and inflame the lymphatic vessels, leading to lymphedema.
- Filariasis: This parasitic infection is most often seen in those who live in tropical regions.
4. Obesity
Obesity is a significant risk factor for secondary lymphedema. Excess adipose or fatty tissue can compress heavily on lymphatic vessels, leading to compression of lymphatic vessels and nodes or permanent damage. Morbid obesity has the potential to cause secondary lymphedema that becomes chronic, meaning even if one loses weight, the damage to the lymphatics remains and is no longer reversible, leaving one with lymphedema lifelong. A body mass index above 30 does increase the risk of localized fluid buildup. It’s suggested that obesity-induced lymphedema occurs in those with a BMI above 53.
Obesity can also contribute to systemic inflammation, which can exacerbate swelling. Along with the compression and damage, obesity often leads to lower physical activity. Reduced movement can cause further pooling of lymphatic fluid and worsen lymphedema symptoms.
5. Prolonged Immobility and Medical Conditions
Extended periods of immobility, such as being bedridden after a medical issue or paralysis, can lead to fluid buildup.
- Post-Surgical or Illness: If someone is bedbound for extended periods of time to heal from surgery or a severe illness, this can lead to stagnant fluid flow, especially in the legs. Not only does this increase the risk of lymphatic fluid buildup, but it also increases the risk of a blood clot.
- Paralysis or Stroke: Conditions that lead to reduced or lost movement, such as spinal cord injuries or strokes, can contribute to lymphedema by decreasing natural muscle pumping action. The lymphatic system relies on muscles to move fluid through the lymphatic vessels. When muscles cannot be activated, fluid can accumulate in the area.
6. Cardiovascular and Renal Diseases
Heart failure and kidney disease can cause visible swelling and may lead to secondary lymphedema due to increased fluid and pressure placed on the lymphatic system.
- Congestive Heart Failure: Poor cardiac function can cause fluid accumulation in the arms or legs and increased work for the lymphatic system.
- Kidney Disease: When the kidneys fail to regulate or remove excessive fluids, swelling can occur, affecting lymphatic drainage.
- Liver Disease: Conditions like cirrhosis can cause protein imbalances and fluid retention, often seen in the abdomen, which may indirectly affect lymphatic function.
Symptoms of Secondary Lymphedema
Secondary lymphedema may come on gradually, making it vital to monitor for any of these common early symptoms:
- Swelling in a body region, most commonly the arms or legs.
- Heaviness, fullness, or discomfort in an area with or without visible swelling
- Hardening or thickening of the skin (fibrosis)
- Frequent infections such as cellulitis
Unlike general swelling, lymphedema is chronic and progressive, meaning it may worsen over time if left untreated.
Management and Treatment of Secondary Lymphedema
While various medical reasons may cause secondary lymphedema, the treatment and management of symptoms remain similar to that of primary lymphedema and cancer-related secondary lymphedema:
1. Complete Decongestive Therapy (CDT)
CDT is the gold standard for lymphedema treatment with a certified lymphedema therapist and includes:
- Manual Lymphatic Drainage (MLD): A specialized hands-on manual technique that stimulates lymph flow through lymphatic vessels and out of a congested area.
- Compression Therapy: The use of multi-layered compression bandaging to reduce fluid or garments to maintain the reduction of swelling.
- Exercise: Movements can encourage a muscle pump in the body to allow for the natural movement of lymph fluid.
- Skin Care: Proper hygiene, nail care, and skin care are essential to avoid infections such as cellulitis.
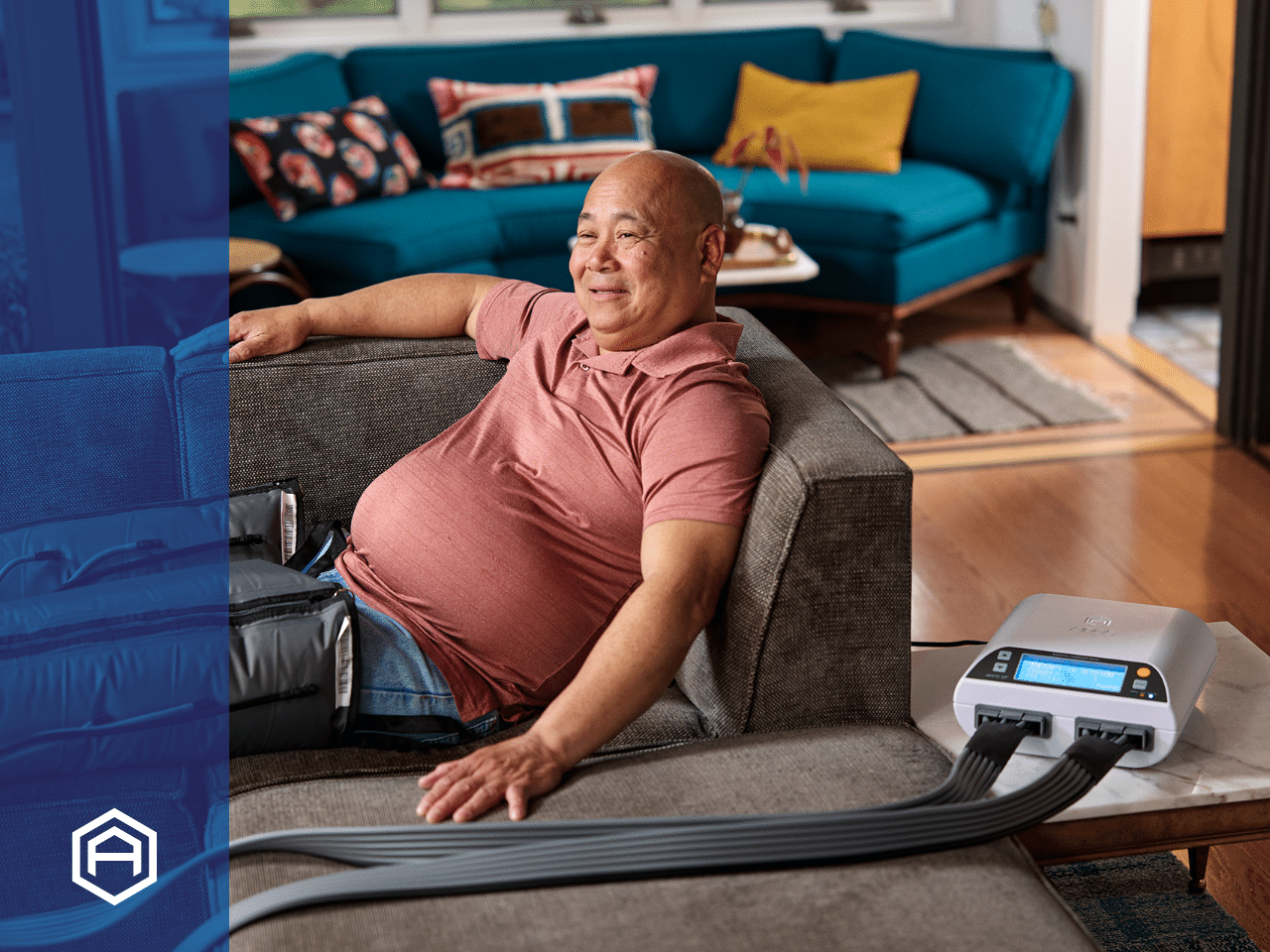
2. Compression Pumps
Compression pumps, or pneumatic compression devices, are great long-term treatment options for moving lymphatic fluid and reducing swelling. They can be used daily at home to minimize swelling and encourage lymphatic fluid flow. They benefit individuals with significant lymphedema who need support beyond MLD and compression. Airos Medical has an entire line of compression devices and garments engineered for ease of use.
3. Physical Activity and Weight Management
Consistent exercise such as walking, swimming, or rebounding can support the lymphatic system by encouraging fluid flow. For individuals with obesity-related lymphedema, weight loss can significantly improve symptoms and reduce pressure on lymphatic vessels.
4. Surgical Options
In severe cases, surgeries such as lymphovenous bypass or suction-assisted liposuction may be an option.
Wrapping it Up
When doctors, healthcare providers, and the general community can understand and identify the various causes of secondary lymphedema, it supports individuals and patients in getting access to appropriate treatment to avoid the progression of lymphedema. By addressing underlying conditions and receiving optimal treatments to manage non-cancer-related secondary lymphedema, those affected can prevent long-term complications and improve their quality of life.
Sources:
Mehrara BJ, Greene AK. Lymphedema and obesity: is there a link?. Plast Reconstr Surg. 2014;134(1):154e-160e. doi:10.1097/PRS.0000000000000268
Vignes, Stéphane, Florence Poizeau, and Alain Dupuy. “Cellulitis risk factors for patients with primary or secondary lymphedema.” Journal of Vascular Surgery: Venous and Lymphatic Disorders 10.1 (2022): 179-185.
Varghese, Smitha Ancy. “Secondary lymphedema: Pathogenesis.” Journal of Skin and Sexually Transmitted Diseases 3.1 (2021): 7-15.