NOTE – EDITED DECEMBER 5, 2024 – The information in this article was originally provided when Medicare’s Local Coverage Determination (LCD L33829) for Pneumatic Compression Devices (PCDs), which provided guidance on billing for these types of devices, was in effect. The LCD L33829 was retired on November 14, 2024, and is no longer in effect. While much of the information below is still relevant, there may be some changes that impact some of these steps. Please contact us directly to get more information and details.
One of the most frequent questions our customer service teams get from physicians, lymphedema therapists, and patients is: “How can a patient get a pneumatic compression device for lymphedema treatment?”
Despite the fact that pneumatic compression devices (PCDs) have been available and covered by Medicare and commercial insurance for decades, many clinicians are still confused about the billing aspects of these important medical devices. While Medicare and commercial insurers change their policies from time to time, there are some basic elements of what is needed for a prescription – or “standard written order,” when working with Medicare.
Below is an overview and some definitions that clinicians we’ve talked to have found useful.
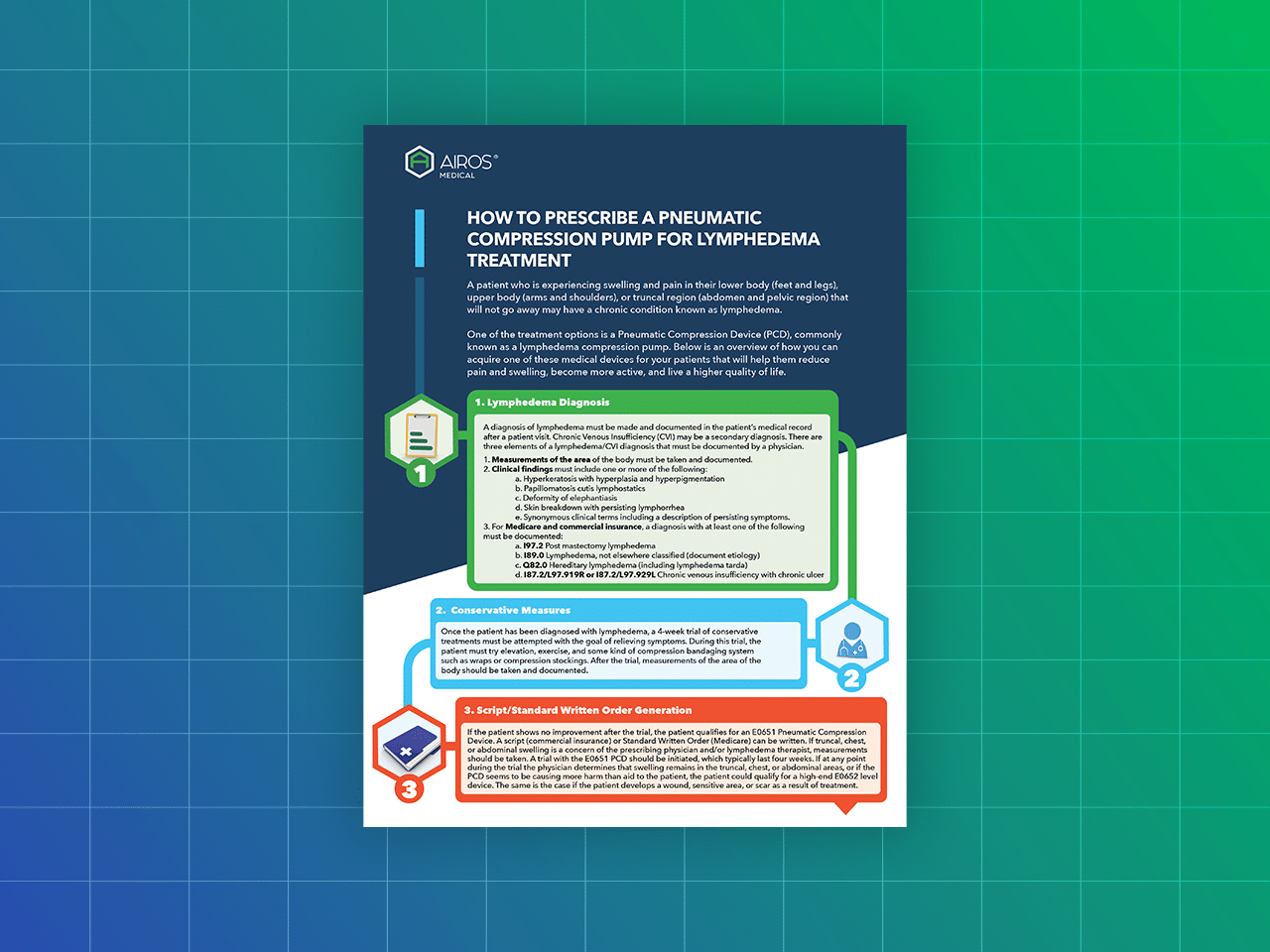
Step 1: Lymphedema Diagnosis
A diagnosis of lymphedema must be made and documented in the patient’s medical record after a patient visit. There are three elements of a lymphedema/CVI diagnosis that must be documented by a physician:
- Measurements of the body area
- Clinical findings, which typically must include one or more of the following: Hyperkeratosis with hyperplasia and hyperpigmentation; Papillomatosis cutis lymphostatics; Deformity of elephantiasis; and/or
Skin breakdown with persisting lymphorrhea - A diagnosis with at least one of the following: Post mastectomy lymphedema; Lymphedema; Hereditary lymphedema; and/or Chronic venous insufficiency with chronic ulcer
Step 2: Conservative Measures
Once the patient has been diagnosed with lymphedema, a 4-week trial of conservative treatments must be attempted with the goal of relieving symptoms. During this trial, the patient must try elevation, exercise, and some kind of compression bandaging system such as wraps or compression stockings. After the trial, measurements of the area of the body should be taken and documented.
This trial must be executed in order for a prescription to be written.
Step 3: Prescription/Standard Written Order
If the patient shows no improvement after the trial, the patient qualifies for a “basic” E0651 Pneumatic Compression Device. A prescription (commercial insurance) or Standard Written Order (Medicare) can be written.
If truncal, chest, or abdominal swelling is a concern of the prescribing physician and/or lymphedema therapist, measurements should be taken. A trial with the E0651 PCD should be initiated, which typically last four weeks.
If at any point during the trial the physician determines that swelling remains in the truncal, chest, or abdominal areas, or if the PCD seems to be causing more harm than aid to the patient, the patient could qualify for a “high-end” E0652 Pneumatic Compression Device. The same is the case if the patient develops a wound, sensitive area, or scar as a result of treatment.
In order for an E0652 device to be acquired, the patient must try the E0651 device. Only a physician can make the determination that the device is not providing sufficient treatment and that a higher end E0652 device is needed. Not every patient requires a high-end E0652 device.
This element of the prescription is typically the most confusing for physicians and lymphedema therapists.
Step 4: Durable Medical Equipment Supplier Fills Order
Once the prescription/standard written order is completed, it can be sent to a Durable Medical Equipment (DME) company that provides pneumatic compression devices for the order to be filled. The DME will work with you and the patient’s insurance company (Medicare or commercial insurance) and will also handle the paperwork and documentation required for billing. The DME may be the device manufacturer itself, or it may be a separate company.
Please contact us if you need help finding a DME in your area.
Step 5: Device Delivery & Patient Treatment
A PCD may be shipped directly to a patient, or a field technician from the DME will deliver the device to the patient’s residence. The DME’s field technician will come to the residence, show the patient how to use the device, have you and the patient complete necessary paperwork.
Next Steps
AIROS Medical’s team has decades of experience providing PCD devices to patients and working with DMEs directly to help lymphedema and CVI patients receive the treatment they need. Please contact us with any questions about this process, or to help you find a DME in your area.